Learn how to balance hormones naturally WITHOUT hormone replacement therapy! Improve skin, reduce belly fat, make menopause bearable, and improve sex drive for men and women of all ages. In my interview with Dr. Garrett Smith, ND we discuss why hormone imbalance is a uniquely modern-day problem, and how removing toxins and replenishing nutritional deficiencies can help our bodies heal.

Life is hard enough…
Yet for the aging woman, entering or having gone through menopause, or even having hormone dysfunction early on in life, it can be even harder still because her sex hormones either drop off completely or are all over the board.
The hormone imbalances in estrogen, progesterone, and testosterone, as well as thyroid hormones, causes older looking and sagging skin, more belly fat, loss of sex drive, trouble sleeping and focusing, hair loss, painful cycles, infertility, and emotions being “all over the place”.
It’s a fact that imbalanced hormones can lead to a painful decline in quality of life.
So, I’m excited to welcome Dr. Garrett Smith from NutritionDetective.com to discuss how to heal and balance hormones naturally.
Dr. Smith is a licensed naturopathic medical doctor in Arizona. He has a Bachelor of Science in Physiology with a minor in Nutrition. He spent 12 years as a strength and conditioning specialist. Yet, when he realized that nutrition was inseparable with fitness, he got into the medical field. His approach is unique because he takes a look at a person’s individual vitamin and mineral metabolisms. He has foundational approaches that tend to help most people, but beyond that, he treats specifically for how an individual’s body functions. Which is really refreshing!
In this interview, we’re going to get into some of those foundational approaches. Specifically, we’re talking most of the time about how his Love Your Liver program can help with hormone balance for men and women of all ages. I have been working with him personally for the last six months and my thyroid medication is down by one-third*. In the previous six years, I have only ever had to increase it! I feel like I have just barely started getting well, and more improvement is yet to come.
*In fact, since recording this interview, I have been able to get off thyroid medication completely, as well as wean off the other bio-identical hormones I was taking (progesterone and testosterone).
If you or someone you know struggles with hormone imbalance… then please listen to — or read or watch — this podcast interview with Dr. Garrett Smith from NutritionDetective.com to learn how to treat hormone imbalance… WITHOUT taking supplemental hormones, bio-identical or otherwise.
This is a different message than I’ve shared before, I know. My husband and I have both had ups and downs with bio-identical hormone replacement therapy (BHRT). We started on BHRT over six years ago (at the time of this interview). For me, at first, I felt they helped some of my issues. But at some point, I started getting unpleasant side effects like headaches, dizziness, and fatigue. Increasing the dosages just made those things worse or didn’t help them… and I developed “new” issues. For my husband, they may have helped him a little from time to time, but ultimately, they barely touched his original issues.
So we are both happy to look at healing the underlying causes, such as toxicities and deficiencies, that Dr. Smith shares in this interview. I’m learning so much, and hope you will learn from it, too.
In this article:
- how hormone imbalance is linked to modern-day toxins and deficiencies
- the best way to balance hormones for men and women
- why hormone replacement therapy, even using bio-identicals, is not the solution to hormonal balance
- testimonials from Dr. Smith’s patients
- and much more!
Please set aside distractions and watch or listen to the video below. Or, if you prefer to read, the complete transcript plus my summary notes are below!
Wardee:
Hey, everyone, welcome. And I'm joined by Dr. Garrett Smith. Hi, Dr. Smith.
Dr. Smith:
Hello.
Wardee:
Thanks for joining us, Dr. Smith and everyone I just want to do a quick introduction of Dr. Smith. He is a naturopathic doctor practicing in Arizona and he's been in the medical field for over 15 years and prior to that, for a dozen years in the fitness and health industry. And I've asked him on today to help us with healing hormones. And for women and men in our audience, hormones are a huge problem and I asked Dr. Smith to come on today and give us a peek into why we're having these problems and natural healing approaches for them. So it's going to be a great interview. I'm looking forward to learning a lot and so thanks, Dr. Smith.
Dr. Smith:
Happy to be here, glad I could make it.
Wardee:
Me too. So why don't you start by telling us a little bit more of your background information so people can get to know you a bit.
Dr. Smith:
Okay. Like you said, I was in the personal training field. I originally, as a kid, got into bodybuilding and lifting weights. And that eventually leads to nutrition because as they say, what? 90 percent of fitness is in the kitchen, right? So fitness lead to nutrition. Nutrition lead to naturopathic medical school and that lead to where we are now.
Dr. Smith:
I did a bunch of approaches in my past. I had phases like most MDs do or alternative practitioners do where they think everything's caused by this one thing. Whether it's candida or toxic metals or Roundup or whatever. Hormone deficiency, right? That's out there, too. Everybody's like well all your problems are caused by a hormone deficiency so if you just take hormones, then we can fix it. So I was always looking for what I would consider to be the skeleton key, if you will, to unlocking ... I always felt like there has to be something in common between all of these things. What are we all doing wrong on some level that is causing us these chronic diseases? It may show up differently in different people which always made sense to me as why do colds and flues, why does one person have a sore throat and another person doesn't? Why does one person have a fever and another person doesn't? So it's supposedly the same thing happening but it shows up differently in different people. So can chronic disease do exactly the same thing? Could it be the same cause, general causes, but showing up differently in different people?
Dr. Smith:
So philosophically, I was always trying to get to the root of things. One of our oaths is treat the root cause, treat the cause. And I saw my fellow practitioners, the people I went to school with, doing things like Botox and things like prolotherapy where they're injecting into joints which is not a bad thing. A lot of things that treat symptoms are not necessarily a bad thing. But if we can figure out what is causing the problem and we can remove that ... Let's just say it's a toxicity causing the problem. If we can remove that toxicity, the body can fix the damage. In my estimation, if we give it enough time. If it's a mineral deficiency, then we can give the body what it needs and it can refill its stores and then it can do what it wasn't doing before.
Dr. Smith:
So those several things is what drove me, that's what I figured out was kind of the root of most people's problem and that's what I do like we're going to talk about today in terms of hormone issues is we're working on fixing those things. So that's where I'm coming from.
Wardee:
Great. I love that. And that really corresponds to your name online, Nutrition Detective looking for toxicities and deficiencies.
Dr. Smith:
Yes.
Wardee:
And everybody's individual. I think it's such a great approach because this isn't cookie-cutter. It's like what's going on in your body?
Dr. Smith:
Yes.
Wardee:
Fantastic. Okay. So here's a big question for you. Why do we have hormone problems?
Dr. Smith:
Why? That's a big question.
Wardee:
Yeah.
Dr. Smith:
How do these things start. Well I was going over today in terms of ... Because hormones is a big category. There's sex hormones, there's thyroid hormones, there's adrenal hormones, there's all these hormones in different areas.
Dr. Smith:
So I was going over everything on my livestream on YouTube about the connections between how Vitamin A, which one of my expertise areas is in Vitamin A toxicity. And how Vitamin A toxicity can negatively affect thyroid hormones. For those of you who are unfamiliar with me, I do not believe Vitamin A is a true vitamin. I believe that it's derived from a plant poison called carotenoids. And I help people get better by having them avoid it.
Dr. Smith:
And as an example, a lot of ladies out there are often told that they're estrogen dominant. They have too much estrogen relative to progesterone. Well two of the big things that I treat ... Many people, hopefully, are familiar with plastics and plasticizers that are toxic to humans and animals. And they're very, very estrogenic. So we have this toxicity problem right off the bat. We have estrogenic toxicity from things that are, they're called xenoestrongens which are ... If you think of the word xeno as being alien, they're alien to our system. They're not meant to be in our system and they maybe weren't really meant to be on Earth until we made them. So xenoestrogens is one. One of the things I tell people not to do too much is what are called polyphenols which is where plant phytoestrogens come from. And so people are eating lots of plant estrogens. Most people are familiar with these things from soya beans. And many people out there are very familiar with soy as not being a really good thing to consume and soy contains anywhere from 1000 to 10,000 more phytoestrogens than other plants.
Dr. Smith:
When they ferment soil, like tamari or tempeh or natto or the fermented soy that was very traditional in traditional Japan, that actually destroys most of the phytoestrogens. Why did they start doing that? Why would they take more effort, put more effort, into preparing their food unless it was probably for a good reason? So we have phytoestrogens.
Dr. Smith:
And then we get into things like Vitamin A. Vitamin A is actually ... I could put my little quotes around it. It could be like "Vitamin", because it's not really a vitamin in my opinion. But it's very estrogenic. It stimulates aromatase activity which is what converts testosterone into estrogen. And so we have that effect.
Dr. Smith:
One of the other things I treat in people a lot is copper toxicity. Copper toxicity, which especially ladies, if you've done things like birth control pills. I have a video on my YouTube about how birth control pills will raise Vitamin A and copper in the bloodstream and they've known this since 1975. So we know that it's retaining more Vitamin A and copper in you. And the funny thing is, what you're hearing me say is Vitamin A's not good for you and copper's not good for you. And birth control pills are effectively making you infertile. And we just coincidentally see Vitamin A and copper raising in your system. And then we also see a copper IUD. So they actually stick a copper wire inside of you and it makes you infertile. So these things absolutely affect your hormones and your fertility and I've talked before about how fertility is health and health is fertility. So if you damage your fertility, whether you think it's temporary or not, you are damaging your health.
Dr. Smith:
So those things, copper is extremely estrogenic. If you wanted to think in terms of masculine and feminine or testosterone and estrogen, copper is extremely estrogenic and Zinc is the antagonist of copper and Zinc is pro-testosterone which everybody needs. Don't think that just women need estrogen and men need testosterone. It's not that clear-cut. We all need some of both of them. But in our world today, everything is very radically geared towards excess copper, excess Vitamin A, not enough Zinc, plastics. Many toxins are very estrogenic. But we just tend to get this overload of estrogens and these things that are often estrogenic can be stored in our fat. If they don't go away right away, they can be stored in our liver, they can be stored in our fat. And so they sit there and as long as ... If you're taking in more in a day than your body's able to get rid of, you are slowly accumulating them and your problems will slowly get worse over time. It's just math, as they say.
Dr. Smith:
So yeah, that's where a lot of it comes from. That's where I fix. I have a video on my YouTube about my recent ... I'm 46 and my recent testosterone was basically about 900 which is for a 46-year-old man, small business owner, two kids, that's really, really good. And I do nothing special to ... I don't boost my testosterone. I don't ... I'm not taking testosterone, I'm not using testosterone boosting herbs, I'm not doing any of the stuff that all the internet people are trying to sell to people. So what we're doing ... And I have lots of women who, we'll go over testimonials towards the end, I think. I have lots of women who have gotten hormone situations better with enough time. This is not a quick fix. Fixing root causes takes time. It's a marathon, not a sprint.
Dr. Smith:
But yeah, I think we covered that. I think we did.
Wardee:
Yeah. So if toxicities like Vitamin A, copper, phytoestrogen or plants-
Dr. Smith:
Phytoestrogens are one, yes.
Wardee:
Mm-hmm. And so that leads to estrogenic effects in men and women?
Dr. Smith:
Yes, typically estrogenic effects.
Wardee:
And so things then get out of whack.
Dr. Smith:
Yes. And so if you either add estrogens to the system, obviously that's estrogenic in some manner. And then if you increase the activity of what's called aromatase which is the enzyme that can turn testosterone into estrogen, which is one thing that Vitamin A has been shown to do in the research, then you're simply taking a hormone that your body wanted there, like testosterone, it made it, and then these toxins, if you will, are turning them into estrogens.
Wardee:
Okay, wow.
Dr. Smith:
And then there's the estrogen dominance theory which is not enough progesterone relative to estrogen. So you're getting a dominant estrogen effect which is then causing a lot of issues. Estrogen is a very tissue growth oriented hormone. Estrogen causes tissue growth. This tends to cause fat, more fat, more body fat. Which is why in general, women have more estrogen than men. This is why, I try to say this in the nicest way possible, women are smoother than men. Women have more body fat than men. Part of that's for childbirth, childbearing, childbirth and all that stuff. But women just have more estrogen and estrogen tends to make more body fat.
Dr. Smith:
Estrogen, the areas ... If you start getting estrogen out of control, one area of the body, especially in women that's very controlled by estrogen is the breasts. We have an epidemic of breast cancer. We have epidemic of excess estrogens. This all seems to start sitting together. And there's lots of other sexual organ cancers and tumors like fibrocystic disease. When you think of tissue growth, especially out of control tissue growth, think estrogen. It's just something to automatically go to. Why is there more estrogen?
Dr. Smith:
And then, as an example, when I say that copper is very estrogenic, when you start looking into cancer research and you see the tumors are higher in copper than the other tissues around them, it starts to fit together. Just estrogen likes to grow tissue. And when people, especially ... I mean men or women, when they get too much estrogen you can usually see they start gaining body fat because estrogen just makes more body fat. Body fat contains aromatase. So then any of the testosterone you're making hits that body fat, it gets turned into estrogen, estrogen makes more body fat, and you get this really vicious cycle.
Dr. Smith:
And then again, the soils are deficient in things like Zinc and molybdenum which are the antagonists to copper and Vitamin A. And so you're not getting in enough of these critical minerals to regulate things and you're getting too much of these other things. I mean people don't realize their tap water and their shower is full of copper most times because we have copper water pipes going to and from our water heaters. So you're absorbing that copper. Don't let anybody tell you you're not absorbing that copper from your shower because I can see it on hair tests. I have people who react to showers. Once they start paying attention, they're like, "Oh my gosh, I had no idea I felt so bad after my shower why that was and now I know it and I know that ..." They actually are doing science stuff. Some people are avoiding their shower tap water so much because of the copper because they feel better when they do it, when they avoid it. They're doing the old Irish shower-
Wardee:
Sponge bath.
Dr. Smith:
With a dish, with a towel. And they're just washing themselves outside the shower with as minimal water as they can. They're even using reverse osmosis water to do these little bathing episodes. And they feel better doing them. So this copper thing is a really big deal.
Dr. Smith:
And then you have other people out there who make supplements and who push supplements saying if you're going to take a Zinc supplement, you have to take copper with it. And I'm going, "No, no you don't." I mean every time you add gas to your car, you don't have to add oil. You don't add oil every time we add gas. Do we need both of them? Yes, but we add gas tons of times before we have to change the oil. So it becomes a really big deal.
Dr. Smith:
And then especially for the ladies listening, if you have a chocolate addiction, that's copper toxicity guaranteed. Chocolate is super high in copper and no one ever said that people ... That's an example people say. "But I like chocolate so much. Why would I like it so much if it was bad for me?" And I go, "Drug addicts love drugs." They don't take the drugs because they don't like the drugs. They take the drugs because of how it makes them feel. Well lots of other things, coffee, chocolate, all sorts of these things that we use or that we take, we do it because it makes us feel a certain way. That's not necessarily good for us. But chocolate's huge on the copper front. And I have lots of women come to me especially who are totally addicted to chocolate and I'm like, "We got to get that down or get that out to get you better." And that's why this is not easy. What I do is not easy. I never said it was. But I think those are some of the big things.
Wardee:
Okay, okay. So before we start talking about solutions, it takes time, talk to us about menopause in relation to ... There's normal hormones, then we have hormone issues from toxicities. But then there's menopause, when our body's hormone production decline. So how does that fit into the picture? What's your view on menopause?
Dr. Smith:
What is my view on menopause? So the thing to remember is that the ovaries are not the only hormone producers in the body. The uterus makes hormones, the adrenal glands make some sex hormones. We have other ... Body fat makes estrogen. I mean the thing I always thought about that I always thought was interesting was how they say we have ... You know how they neuter ... Neutering is male dogs, right? I'm just ... Spaying is female, neutering is male, right?
Wardee:
Mm-hmm.
Dr. Smith:
So you know how ... They chop off a dog's testicles. And the dog lives. I mean the dog doesn't keel over and die. So obviously it still has some testosterone and I have a dog, it seems to have a decent amount of muscle. But it has no testicles. So part of me is, with the whole menopause thing, I mean yes the ovaries can stop producing but we're still making hormones. We're not ... We don't die of a hormone deficiency immediately. Shouldn't that happen pretty soon if that was the only thing that made hormones? They still run blood tests, we still have hormones. But obviously if they go and they remove let's say the uterus as well and the full hysterectomy, that's going to be ... Because the uterus does make quite a bit of hormones and this is in the literature.
Dr. Smith:
Ladies, if you're out there and your doctor says, "Well, your ovaries are gone, you're not making hormones anymore," they're not up on the science because the uterus makes tons of hormones. And the adrenals make sex hormones and the body fat makes estrogen which is a sex hormone. So you're not not making anything anymore.
Dr. Smith:
Now interesting things about ... I mean here's ... How does the whole menopause thing work? You got to remember what I do is I'm just trying to get people, get rid of the toxicity and fix the deficiencies. That's what I do. We have had women who were in menopause start cycling again. What did I do? I didn't do that people would be like, well how did you make that happen? And a lot of women are like, well I'd rather not cycle anymore. Not really interested in having babies and I'm going, well cycling is youthful. If you want to be more youthful, you might want the more hormones of youth which would mean you want to cycle, in a way. So I'm just trying to explain it as like it's yes, it may be a pain in the butt ... Not that I'm familiar with it. I've never had to deal with that myself. But it might be a pain in the butt, but you are healthy. So all I was trying to do was make them healthier. I had no idea that this would happen and it happened.
Dr. Smith:
But another thing that we deal with in terms of, you know how I said the adrenal glands make sex hormones? And I've talked about Vitamin A toxicity. Well, it's in the literature, it's in the scientific literature that they have used retinoic acid, the same chemical as Retin-A or tretinoin, some of you ladies may be applying this to your face and absolutely destroying your liver. Your face may look great but your liver is suffering. They gave this to people and these people had Cushing's syndrome which is hypercortisolism. So their adrenal glands were producing ... And it's an autoimmune condition. Their adrenal glands were producing cortisol overtime, too much. So they were getting symptoms of excess cortisol or cortisone. They were getting the moon face and all the things that go with taking too much corticosteroids.
Dr. Smith:
Well, they used the retinoic acid, the active form of Vitamin A, that when you eat Vitamin A in foods, some of it eventually turns into this stuff. They used this to shut down the adrenals so lower the cortisol production. So for those of you out there who are into alternative health and you've learned about adrenal fatigue, I'm telling you that they use active Vitamin A in studies to basically induce adrenal fatigue. So imagine if you had hyper-adrenals and you then give retinoic acid to drive them back down to more normal, then what happens when you have normal adrenals and then you drive them further down? Wouldn't that be adrenal fatigue?
Dr. Smith:
And what am I having people do? Avoid or reduce or minimize Vitamin A and then we're seeing things like women's cycles starting again. And now we have ... I have another woman DEXA scan's tested, shown that she has started ... She was osteoporosis, getting worse every year. And all of a sudden, we turned it around. We actually reversed ... She was actually building bone. [inaudible 00:20:51]-
Wardee:
So you're saying-
Dr. Smith:
Sorry, go ahead.
Wardee:
... you're starting to see evidence of menopause, the supposed menopause symptoms, not being so bad or being reversed when you correct nutritional deficiencies?
Dr. Smith:
Absolutely, absolutely. Menopause was never ... Pregnancy and delivery was never meant to be the hell that it's become for women these days because they're sick.
Wardee:
Agreed.
Dr. Smith:
As an example. And I have women tell me that the kids they have, after they started working with me, pregnancies were easier, deliveries were easier, kids come out healthier than their other kids, often. And then we look at menopause and menopause, I get women with hot flashes and we get them out of hot flashes. We are not designed to suffer through these things. We have way created these problems and now they want, the bad guys, want us to normalize it so that we just think it's normal that life just sucks because they're not going to give us the nutrients we need.
Dr. Smith:
I saw a paper, it said that 50 percent of the soils in China were Zinc-deficient. 50 percent of the soils in China. Now people will say, "Well, China." Maybe they assume that China doesn't always tell the truth. Okay, so if they're saying, if they're letting out the data that 50 percent of the soils are Zinc-deficient, is it 80 percent? Is it 90 percent? Is it 100 percent? So then you start going, okay. And then what do they want us to do? What's the best source of Zinc in food? It's red meat. Is there a concerted effort to get everybody to eat less red meat right now?
Wardee:
Yes.
Dr. Smith:
Seems like it to me. So ...
Wardee:
Okay, well that is shocking.
Dr. Smith:
Yeah. There's a lot of funky stuff going on right now.
Wardee:
Yeah. Well I was saying shocking about what you just said, just calling into question whether what we know about menopause is actually normal. So there are definitely bears watching.
Dr. Smith:
Yeah. What I think what women are going through is not meant to be. What we've been told to think is normal of the hot flashes and the osteoporosis and all this stuff. I have a paper on osteoporosis where they showed that generally when people got more than 3000 units of Vitamin A a day, their osteoporosis was worse. Well a lot of people who are trying to eat healthy diets, they might get 3000 units of Vitamin A with breakfast. And that's not even including their lunch and their dinner of sweet potatoes and whatever. So it's-
Wardee:
And then their multivitamin.
Dr. Smith:
Yeah. And then they add their multivitamin and then they add their super foods, basically. If you're out there eating a super food that's sold to you as a super food, it's super high in Vitamin A. It's tragic and I'm out here trying to undo it. [inaudible 00:23:59].
Wardee:
Okay. So speaking of trying to undo it, what would you say about what's the best way for people to balance or fix their hormones? And you can speak generally but it would also be great if you would address women and men individually or specifically.
Dr. Smith:
Well the funny thing about addressing women or men specifically is ... Well as an example, when people work with me directly, so there's two ways that people know that I work with people. One is the Love Your Liver Program which is a do it yourself thing. That's my diet and toxin avoidance and there's some general stuff on there on supplements. And then there's people who work with me directly which is where we do the blood and the hair testing so that I can give ... And there's the followup so we can guide people to getting what they need for them. Because some people, like with Zinc, some people are amazingly sensitive to Zinc and they can hardly take any or maybe they don't take any at the start. And then some people are on a lot of Zinc. And they're coming in weekly to my support groups where I'm monitoring. They're giving me feedback and we're talking about it and we're seeing how things are going so we can decide what to do next.
Dr. Smith:
So in terms of ... Honestly, I don't have different approaches for men and women because toxins are toxins. There's not male-specific toxins and female-specific toxins. I do know one example that I've heard of but this is just one. Polyester in your underwear in men will reduce your testosterone and your sperm count. So wear cotton underwear, basically. So would I say that that's probably extending to women as well, why not? If it affects men like this, why would it not affect women too? It might just be the amount of skin touching it might be more for men than women. That might be a difference and that's where they see it.
Dr. Smith:
But in terms of, let's say the major minerals that I work on with people with Magnesium and Zinc and Selenium and Molybdenum. The only thing that changes on those, other than ... The only thing that changes ... There's their reaction. There's what their tests say. There's their body weight as a guiding thing. There's their history of how they've reacted to these things. And these are all the things that I take into account as I work with somebody to make the approach fit them. And somebody might be like, well you said Zinc was pro-testosterone, why are you going to give it to women? Well I have a lot of women coming in with too much estrogen. And do I test hormones? No, we can just look at symptoms for the most part. Hormone testing, as many of the people out there will know, it's very, very expensive. You get a couple tests and you're up into hundreds of dollars of testing.
Dr. Smith:
So the hormones themselves ... So here's a different concept. I think of hormones as a symptom. People will say, well hormones are the top of the pyramid. They're the most powerful things in our body. They're the most important. I go, okay. So if they're at the top of the pyramid, right up here, what are they built on? They're built on everything below. So if you're talking about toxins at the bottom and then you got minerals above that. And then you've got, let's say, I don't know, protein and other macros above that. And you're just going, okay exercise. Okay, exercise is going to affect your hormones but if hormones are the top of the pyramid, they're built on everything below it. And if I'm right, then that would explain my good testosterone now because what I'm working on is everything below it and I'm not having to take testosterone.
Dr. Smith:
And just so people understand, I used to give testosterone replacement therapy in my practice. I used to have quite a few men in my practice where I was doing testosterone therapy and I was very good at it. I learned about testosterone just like I learned all about nutrition later. I just decided at some point, philosophically, in my heart, I said, "I'm not treating the cause." I want to treat the cause and at some point I decided that I needed to ... I didn't want to give hormones at the same time as I was giving nutrition because it seemed like I was going, well what's fixing what and how do I tell?
Dr. Smith:
As an example, let me give, some of the ladies out there who have done hormones will relate to this because this is mainly what I noticed in guys but this would absolutely extend to women. So if you go to the doctor and they say, "Okay, we tested you. We looked at your symptoms, we tested you, you need X amount of estrogens." The E1, E2, E3, whatever they're doing. "You need so much progesterone and maybe we'll add a little testosterone in the mix." And they start using it. And they get a honeymoon phase, they feel great, sometimes. Sometimes they feel worse. Sometimes they feel ... Most of the time they feel great and they go, "This is great. I got my libido back and everything's working better." And all this stuff, okay.
Dr. Smith:
And they keep using it. I mean they're going to their doctor and the doctor's saying, "Your labs are good, your labs are good. Let's raise you here. Let's lower you here." Or whatever. And they're just trying to maintain what I would consider the symptoms. They're treating the symptoms. People are going in there saying I have these symptoms, doc. And they test them and they say, "Okay, here's your medicine to treat your symptoms." Even if they're bioidentical which is bioidentical is better. Don't get me wrong. Nobody wants those horse piss hormones which is Premarin and all the other synthetic garbage that they just make so they can get a patent on it. They don't care about what it does to you long-term, they just want patent. So they're giving this and so it covers up the symptoms.
Dr. Smith:
So let's say there was a toxicity problem that was a cause of these low hormones. Or, and/or, let's say there's a nutrient problem, like a mineral problem that's a part of the cause of this hormone problem. What happens over time if somebody doesn't figure out what the root cause of the problem is ... Like let's say somebody has a Zinc deficiency in their diet. Over time, if they don't know that that's there, it's likely that that problem is just going to slowly get worse and worse and worse and worse. What happens over time with this in terms of the real world with the doctor? Well the person's saying, "My symptoms are coming back, doc." And the doctor's going, "Oh yeah, your hormones are maybe dropping a little bit. Let's give you some more." And the person ... But they're not addressing the Zinc and so the person maybe feels a little better but they never feel as good as they did the first honeymoon phase.
Dr. Smith:
And they just keep running this same routine where they may be going, they get a little bit adjusted. With guys, you give them testosterone, you take them up fairly high in the normal range. And the guy comes in and he's like, "Hey, doc, I feel good but I'm not functioning as well as I was down there, if you know what I mean. Can we bump it up?" Or whatever. And the doctor will keep raising it until they get right to the edge of the okay range or maybe a little bit above it and the doctor says, "Look, I can't take you up anymore. We're getting into taking steroids range." That's not good for their license to be caught raising guys above the normal range. They're in danger there. So they say, "Look, I don't know why you don't feel as good as you did before but I can't give you anymore."
Dr. Smith:
And so this is a common thing because the body adapts. The external hormones are not the same as the internal hormones. Your body's not in control of them. So over time, their Zinc has been going down. Their selenium's been going down. Their molybdenum's been going down. Maybe they've been getting some magnesium, probably doing pills which are not as effective as topical. Maybe that's going down. Doesn't really matter what's going down, they're not addressing it. And maybe they're just eating fast food all the time, eating tons of garbage, soy bean oil, and seed oils, and eating it out of styrofoam and plastics and they're doing the same stuff because they got the easy way out. They got the hormones which made them feel good.
Dr. Smith:
And then all of a sudden, let's say a lot of these people, at some point they start getting into natural medicine because they go, "I want to get off my hormones." And then they try to get off of them. And they come off of them and they're like, "Oh my gosh, I'm worse than when I started." Now they're wondering why and I'm going, I know why. You got more toxic and more deficient while you put that giant hormone bandaid on to cover it up. Which is ... There's nothing wrong with symptom relief but you have to ... I understand that underneath it, whatever was driving the symptom either has to be resolved or it's very likely just going to fester and worsen over time. So that is what really drives me.
Dr. Smith:
And the difference between men and women, like I said, toxins are toxins and minerals are minerals and we're just trying to get people less toxic and more mineral replete as we might say. So ... Yeah, it's all the same in a way. It's all the same but ... It's the same but different, as they say.
Wardee:
Yeah. And it sounds simple but it also takes time.
Dr. Smith:
It is ... Yes. Simple but not easy.
Wardee:
But not easy. Yeah. Yeah, great. That was a wonderful answer. You got into one of my other questions. Did you want to add anything else about the problems with supplementing hormones, even bioidentical? Is there anything you'd add there?
Dr. Smith:
There is. So for people who are doing ... I think the higher doses of progesterone, there is ... I would highly suggest you go and you Google progesterone toxicity because we do store hormones in our fat and progesterone toxicity is a very legit thing and some of the doctors out there are giving ... The common bigger dose of progesterone, I think it's 200 milligrams if I recall correctly. I'm just not in that world.
Wardee:
I think that's common.
Dr. Smith:
Over time, that can be ... I mean just think about it. If you're taking in more progesterone each day ... Your liver has to process hormones. Hormones are some of the most challenging things. Like these giant intricate things. They're huge compared to other molecules. Your liver has to deal with things. It makes more work for your liver. So if you're taking anything in more than your liver can get rid of, you're going to start accumulating them. Your body doesn't want too much progesterone in your bloodstream so what's it going to do? It's going to shove it into the fat because it can be stored in fat. And then it's people start getting some issues and we start going, well maybe the progesterone's causing you some problems. And then they get off of it. Well you still have potentially months or even years worth of progesterone in your fat cells to come out.
Dr. Smith:
Now, synthetic hormones are just ... Those are just scary. Those are just really ... I did a survey on my Twitter where I was asking women did birth control pills, after you were done with birth control pills, was your health ... I don't remember exactly how I worded it but never the same after that. And I think it was two-thirds of the women who answered the survey said my health was never the same after birth control pills. Synthetic hormones are a disaster. Bioidentical hormones are much better but still you're adding a load to your liver. The more load you add to your liver over time, the more potential liver injury you cause, the slower your liver runs which means you clear even less hormones. Which means it becomes easier to accumulate them and then put them places.
Dr. Smith:
The thing that scares me the most, honestly, is those pellets or those tubes they put in people where it's the time release hormones. Those I thought about, when I was getting into hormones, I thought about doing that. And then I just thought, what if I give somebody the wrong dose or they react badly to them? I was asking the people who were going to teach me how to do this. I was like, what do you do? If they're having a bad reaction, what do you do? And they were like, well there's not really much you can do except they could go get them surgically removed but they have to go and fish around for them. And I was like, oh my God, no. No way am I doing that. That freaked me out. I just ...
Wardee:
So could you clarify-
Dr. Smith:
The issues of ... Sorry.
Wardee:
Could you just clarify since you were just talking about the liver? So creams, pellets, injections, oral, if there's any other forms, they all go through the liver? So they're all hard on the liver?
Dr. Smith:
Yes. Let me explain that real quick. So if you were to take a pill, those go through what's called first pass metabolism which is where you're absorbing the hormones from that pill and they're being absorbed from your intestine. They're going through the liver and the liver has the first shot at them before they've gotten into the ... So the liver's circulation ...
Dr. Smith:
Let me just simplify this. Your guys have a specific circulation that goes right to your liver. So when you absorb stuff out of your guts, it enters the portal vein, the portal venous system. But basically, just think of that as a closed system and it goes right to the liver. It's like the bouncer at a nightclub. You want stuff you're eating and absorbing to go through the liver which is your bouncer. It's going to say, you get to go in, you don't. Okay. So then your liver can chop up a lot of those hormones, which is funny that your liver would chop up a bunch of the hormones. Why would it be doing that if it didn't want to before they reach the system? So your liver will destroy a lot of the hormones that you take orally which is why they have to give higher doses orally. It's also why when men take steroids in tablets, the anabolic and all that stuff, that's why it'll just ruin the livers because they have to put stuff on the hormone so more of it will make it through the liver. But that stuff they add to the hormone damages the liver.
Dr. Smith:
So pills are always, those are going to be the hardest on the liver by far. Anything that comes in from outside of basically the oral route, basically the swallowing route, whether it's creams or whether it's injections or whether it's pellets, those bypass what's called the first pass metabolism because they go right into the bloodstream. Which means, in a way, that your body has even less control over them. They come in through the backdoor. They're basically sneaking around the liver. We figured out ways to sneak them around the liver. So you take more control of your detox away from the liver. So in theory, that could cause potentially more problems because the hormones are in there doing what they do before your liver gets a chance to say yay or nay.
Dr. Smith:
All of it is a load on your liver. If you're out there taking 5, 10, 20, 30, 50 pills a day, plus hormones, your liver has to deal with all of that plus whatever toxicity you're putting in. Plus it has to deal with it in terms of a nutrient deficiency that you may or may not know you have. And it becomes the more things you put into your liver, just think of it like it's your house. The more chores you have to do, the more likely you are to fall beyond if you make any mistake or if something pops up. You get a stomach bug and all of a sudden you lose half a day and you didn't catch up on your chores. Well you still got to do them, it's just harder now and it's more work. And then if you keep falling behind, you keep falling behind. And what that means in your body is if you don't detox stuff, you build up stuff in your blood or your body shoves it into your tissues and stores it so that you have to deal with it later while it damages the very tissues it's sitting in.
Wardee:
Yeah, okay. So it's all load for the liver, oral, direct, direct high load, okay.
Dr. Smith:
And everything we take in is a load for the liver. That's why we want to make sure we're not adding things we don't need and we're getting in ... We're trying to only take in the things we do need.
Dr. Smith:
Just one quick example of that, when people take B Vitamins. I have them do them one at a time and to test them to see. The B complex is a nonsensical fantasy thing that you have to take in all the B vitamins at the same time. Because no food has the magical B complex numbers in it. And some foods don't have hardly any of one of the B vitamins and so it doesn't have really the B complex in it. The B complex is something that was made up, honestly.
Dr. Smith:
But I have people do them one at a time to figure out which of the B vitamins, if any, benefit them. And the ones that don't benefit them noticeably, they stop taking them because otherwise it's just a load for the liver that is not obviously showing benefit. And when I have people eat mussel meat, mussel meat is the highest source of B vitamins you can generally get. So hopefully we get enough of that that we don't have to supplement anything of the B vitamin category. But some people do benefit from it and that's something that has to be completely experimented with.
Wardee:
Women tend to have problems not only with menopause but heading into menopause. So is there anything you'd add there or is that just because we're not normal anymore, we're below normal from toxins and deficiencies?
Dr. Smith:
[inaudible 00:42:46], I won't get into cholestasis and the toxic bile theory today. That's a little bit much for this session perhaps.
Wardee:
Just wet our appetite.
Dr. Smith:
Yeah, yeah, yeah. It's all connected. The coolest thing and a thing that can confuse people about what I do is we work on the same things regardless. We're working on the very same things, just trying to fix these specific ... I mean it would be great to address all the toxicities that are around but still, you've been in my program and you know that it's a lot of stuff. I mean it's not a couple of things. It's not like people will be just like eat organic and avoid Roundup. That's great, that's true, awesome. But it's not as simple as some people out there.
Dr. Smith:
There's a saying I love which is the confidence of amateurs is the enemy of professionals. So when other people are out there on the internet and they're like, "This is the one thing that's causing all the problems." I'm like, "Oh, you're cute. You're really cute."
Dr. Smith:
So it's a lot of things. Some people might think there's a concerted effort to make people unhealthy, to make people sick, to make people infertile. And if there is, those concerted efforts would be affecting both men and women and so then our efforts would be the same for men and women.
Dr. Smith:
So we just use ... Okay, so when we were talking about cars earlier. Pretty much all the cars on the road except for their weird electric ones, all the cars on the road, gasoline cars, they work the same. So if somebody learns how to fix a car, in general, they learn how to fix a big diesel truck and they learn how to fix a little economy car, once they know the concepts and the principles, and if they have the right parts, then they can fix just about any engine out there. Are they going to use different techniques to get the parts out of the car and put them back in? Are they going to use different fluids? Are they going to use different things? Are they going to do different, slightly different things? They might use a different type of oil for car A versus car B. They might use a different type of gas for car A, for car B. And then you have different parts that fit differently. But it's all the same. It's the same but different.
Dr. Smith:
So when we have the concepts and principles right, we just apply them differently for each person or we do more of this for one person and less of this for another person. And then the same problems get fixed but different. Do different people need different things? Yes. But it's not like we're fixing an airplane versus a car. We're all humans. So we all generally need the same things but does that mean that person gains the same amount of Zinc as person B? Absolutely not. Okay? So that's the gist of it, yeah.
Wardee:
Okay. And I like another thing you said elsewhere about how it's, for a single person, at one point in a time they're at this stage and they need these things. And the next point in time ... Like we're changing and it's a process. So we also have to be a detective about, okay, what do I need today that I didn't need last week? Or what do I need less of today than I needed more of last week?
Dr. Smith:
That can ... Yeah. So as we work on it, yeah. We can see certain people at the start ... Let's say if they're working with me, that I'm feeling out where they are. We might see them at certain points, their needs actually go up as we're testing and we're seeing their body's just basically ... It takes a while ... We only test about once every four to six months. So in that time, things can change. Month seven, their body starts going, whoa. I loved the Zinc, I used it all up. It'd be like somebody brought you something that you really love to eat and they're planning on it lasting you a month and you're like, well I ate it all in two days. It's like the body can do that with minerals that it really needs that we didn't know ... We don't get to see.
Dr. Smith:
The only way you can really know what is in the body or in the liver is to do a biopsy and take a chunk of them out and analyze it and hope you got an area that is representative of the whole thing. Well, nobody's going to do that. That's not what we're going to do. So then we have to wait and see. Let's say they used up all that Zinc you gave them. I've seen this happen. I start giving people Zinc. They weren't taking Zinc before and they're feeling better on the Zinc and they're doing better. But then we run their test again and they're actually lower in Zinc than when we started. And then what do we do then? We just go, okay, you were doing well on the Zinc, you're feeling better, and your body loved it and it just used it all up faster than we were putting in so we just bump up their dose. And then they feel even better. And then over time as they get saturated, as we refill all of these deficiencies, then they start needing less. And that's the way, in my opinion, things should be.
Dr. Smith:
But a lot of people need tons of potassium in their early days.
Wardee:
Oh, that's me.
Dr. Smith:
And then as we get the poisons out, the toxins out, that deplete potassium, Vitamin A, copper, old Vitamin D supplements that they may have been taking which is shown in the research to deplete potassium. As we get those out, they start needing less potassium. And they feel better all the time. So it's very much, to work in my world, people have to take responsibility and actually watch how they're feeling and take actions based on that which I like to think I explain pretty well in the program and definitely when I do my followups with people. They tell me how they feel and I say, "Here, let's try this and let's see how that works." And then we reassess when we need to.
Dr. Smith:
So yeah, it's a process. But that's why what I hate to have people do is, let's say somebody starts out taking Zinc and they actually don't get enough. It's helping them but then they don't retest. And so now all of a sudden, in a way, they're a little more Zinc deficient than they began. But then they go run to another practitioner because they're like, "Wait, now I have this new problem. I'm going to run over here and try this guy or this lady." And they don't deal with ... One practitioner may have helped one thing but gave them another problem. And then the next practitioner may have helped one thing but gave them another problem and their whole progression, it's like these little jumps but it's going downhill. And this is what a lot of people have with alternative practitioners. They get a new problem from each one of them. It's terrible.
Wardee:
Okay. So let's talk now about if somebody has been on supplemental hormones and let's just, unless there's a difference, let's just say they're bioidentical.
Dr. Smith:
That doesn't matter.
Wardee:
Okay. And so they're through the honeymoon phase and now they're starting to feel worse or they're fine but they're hearing what you're saying and saying, "Oh, I'd really like to fix the root cause." So how can you get off the hormones without tanking or how do you do it the right way?
Dr. Smith:
Well if we're talking about ... We're talking about sex hormones here. I'm not going to get into thyroid hormones, any of that stuff right now. That's all whole nother category.
Dr. Smith:
So if somebody was on ... Like I have people who come to me, and this is ... I am a doctor. But if you are not under my care, I am not your doctor so don't come back to me and say Dr. Smith told me to do this because I'm not telling you listening to do any of this. This is what I would consider doing with an active client of mine who is coming to followups and is listening to what I say.
Dr. Smith:
Okay, generally with hormones, if you don't want to have a big crash, you're going to wean. Now, weaning is done at an individual's rate. They determine it. I never tell anybody how fast they have to wean off of something. But one of the first questions I always ask people is first of all, did the hormones change how you felt? And honestly, you would be surprised at how many people are like, "They didn't do anything for me." And I go, "Well then you should be able to just stop. They didn't do anything for you." It'd be like if somebody drank a bunch of coffee and they're like, "I never felt anything." You go, "Well, could stop your coffee habit right now." And they go, "Yeah, I could. I just did." So it's not a big ... If somebody doesn't feel anything from it, if they're like, "No, I feel the same as when I started." Then just stopping them should not be difficult. Or if some people were saying, no, I just felt bad stuff since I started on them, well then, yeah, stop them and the bad stuff should go away.
Dr. Smith:
For people who are on other hormones, usually when I'm working with somebody, I might have them, if they're doing a test run, they might drop it by half the dose. See, we give it a week or two, see how things change. And then after a week or two, they might determine whether or not they want to drop further.
Dr. Smith:
But yeah, that first question of did you actually feel anything when you got on them was huge. And for people who are, they say, "Oh my gosh, the hormones helped me so much." Like I had a woman using, I think it was estriol for some vaginal atrophy and a lack of lubrication. And she was like, "I'm not quitting this." And I was saying, "I didn't tell you to quit." I don't do that to people. People usually come to me and they say, "I really don't want to take this but I still feel like I need to because of symptom X and B and ..." Whatever.
Dr. Smith:
So I say, "Well I'm not here to ..." I joke about it. It's a crutch but I'm not saying that's a bad thing. People can use all sorts of crutches. Like somebody's taking a blood pressure med so that they don't burst a blood vessel in their head, well is it a symptom fixer? Yes. Is it a crutch? Yes. Are we going to yank the blood pressure medication away from them so that they get a stroke? No, that would be stupid.
Dr. Smith:
So with the hormones, really what we do with the ... What I would do with let's say with that woman with the estriol is we just start doing what we do. And over time, I might say, "Would you feel comfortable with trying less?" And the way I am with my clients, the client is either just like, "Sure, yeah, I'll try less." Or maybe they'll say, I already tried less. They might say, "Yeah, I wasn't quite ready for it. It didn't quite ... I wasn't there yet." Or, "Yeah, it was fine. I went to a lower dose and everything was fine."
Dr. Smith:
So that's how ... Honestly, if somebody was on synthetic hormones, like pharmaceutical hormones, I would first move them to bioidenticals. Some people might tend to think I'm black and white, it's like, no hormones or hormones. No. It's like I tell people who are quitting ... If somebody was talking to me about quitting smoking, I'd say first, get off the Circle K cigarettes. Get on the organic cigarettes. Like first, just take out the toxins in your cigarettes and get less toxic tobacco. And then we can start working on it because then at least we've taken out all those nasty chemicals that they've added to it to keep you addicted. So we've removed a lot of addictions and then we're going to make it easier to quit.
Dr. Smith:
So I don't know why more practitioners don't think in the way I do. I don't get it. But we just wean people off as they feel comfortable. Like with thyroid hormone, I'll go into that real quick. I tell people, you don't change your thyroid hormone until you start getting hyperthyroid symptoms because think about it. So if somebody comes to me and they're medicated on thyroid hormone and they've started managing their thyroid symptoms and they feel better. And then we start doing ... So think about it. Their thyroid production was low and then they took thyroid hormones and it brought them up to here. Well, as we start getting them better, their natural thyroid hormone production is going to move up, this one. And now they're getting back to their normal spot. And now they're over-medicated.
Dr. Smith:
So then, what I talk to them about, I prepare them for it, I say, "I want you to know the hyperthyroid symptoms so that if and when they happen to you, you recognize them." Maybe it's on the weekend and I'm not doing my office hours so I'm not following up with you and you're just like why is my heart racing and I have diarrhea and I can't stop thinking about everything all at once. And you go, okay. So they might cut their dose by half and see if within one or two days the symptoms drastically go back to normal. And if they do, then we very simply know that they were over-medicated because we were actually fixing their thyroid. And some people out there are like you can't fix thyroid. Once you're hypothyroid, you're stuck there. And I'm like, that's not how things work in my world.
Dr. Smith:
So those are ideas of how I work with people to get them. I mean if somebody was working with me and they said, "Look." If it was a guy, let's say. He's like, "I love taking testosterone. I love what it does for me in the bedroom. I love what it does for me in the gym. I'm not getting off of it." I'll be like, "Okay. As long as you understand the consequences of your choices, fine, go ahead. I'm not here to tell you how to live your life. But wouldn't it be really cool if you didn't have to inject your butt every week? Wouldn't that be cool? And you don't have to spend an extra $200 a month on basically steroids."
Dr. Smith:
And it gets expensive seeing the hormone doctors. It's not cheap. The office visit isn't cheap. The compounding pharmacy is not cheap. It's-
Wardee:
The labs.
Dr. Smith:
The labs, oh gosh, the labs. And then you have all that. And then let's say somebody wants to work with me to try and fix it, then you still have all that expense and then you have working with me which, I'm not expensive compared to a lot of that stuff. But then now you have to have two doctors to get off of it. So anyway, it's not an easy position to be in. And like I said, people can stay on hormones if they want. I don't fault them that. We're all just trying to get through this life.
Dr. Smith:
But most people would much rather ... The thing about when you decide ... The way I look at it is, unless you're missing the glands that make the hormones, unless you're absolutely missing them or they've been basically destroyed where they make nothing, we can absolutely improve what your body is making. There's usually a problem of why your body's not making them. And so we can at least start to repair that so that you need less hormones. Whereas when people go into it and they just get on hormones, there's that underlying problem that's likely still festering and so at the end of it, not only do they have the extra load that the hormones wore on their liver, there's also the possibility that maybe they were taking too much estrogen. It starts driving cancer processes and all this stuff. But at the end of it, they're also stuck with whatever toxicities and deficiencies were going on at the beginning, maybe new ones.
Dr. Smith:
And so my approach, just like with fertility, like people who go to the fertility clinics, women who go to fertility clinics, they get pumped up on all sorts of drugs. And then they have a kid who is basically the product of all these pharmaceuticals. And so their kid's not going to be healthy and the woman is less healthy than she began because she's been given all this cocktails of drugs. Whereas when women work with me with fertility, I'm making them healthier and then they get pregnant and then they have a healthier baby than often their other kids. So you can end up with the same outcome. You can end up with a baby. But one of them is a healthier situation by nature and one of them is a not healthy, less healthy situation by nature.
Dr. Smith:
I'm not faulting anybody for the choices they made in the past. I made stupid choices in my past. I did testosterone on myself for six months or a year. I did not like where it ended up with me when I was done with it. That was part of the reason I quit doing it because I was like, "I can't give guys this." I didn't come out ... I came out of it bigger, muscle-wise, but fatter, too. And I was definitely more irritable because my liver wasn't happy. In Chinese medicine, the liver is the seat of anger and frustration. This is why they talk about roid rage is because the more damaged your liver gets, the less patience and the more irritable and the more angry a person tends to become. So especially men. Women may become kind of ... Women would tend to go more towards the weepy, the depressed, the anxious. It amplifies which direction the different sexes typically go in. It just amplifies it.
Dr. Smith:
So yeah, that's kind of-
Wardee:
Wow. Really great info, thank you. It's perfect timing for you to share your testosterone testimony.
Dr. Smith:
I mean ... My test was ... You want me to show the video or pull up the labs or-
Wardee:
Well, I can link to the video. I was just hoping you would just share a quick, it was this, you did hormone therapy, then you did this. Then you ... Kind of just [inaudible 01:00:56]-
Dr. Smith:
Yeah. That's on the video. I'm going to go from memory-
Wardee:
Okay, sure.
Dr. Smith:
... on the numbers. So this was about 10 years ago. I think it was 2012 exactly. My testosterone was 600. So this was only one kid deep. I think I was about 600. And then I got on testosterone and I think I raised it ... I raised it a little too high, a little out of the normal range. I think I was at like 1200 or 1300. So I know what, as they say, being on steroids feels like because I was outside of the high range of normal.
Dr. Smith:
And then my more recent testosterone lab, I was at like 893.5. So 10 years on, after doing ... People will say, oh, well taking testosterone could potentially damage your production for good. Well, I'm higher than that. I'm more muscular than I was in college. I have lower body fat than I've had probably since late teens, early 20s. So everything in my system is running better than it used to.
Dr. Smith:
And so yeah, 600 ... I mean 600 was still pretty good. I mean it's better than most guys have, which is sad. Most guys should be where I am on a regular basis. If everything was healthy, they keep watching it, testosterone levels in men just keep going down and they expect them to go down by ... The expected is to go down by a percent per year. That's the expected decline in male testosterone these days. Do I think that's normal? No, absolutely I don't think it's normal.
Dr. Smith:
My estrogen level, based on the estrogen levels that doctors want who give testosterone, because when you give testosterone, a fair bit of it will turn into estrogen. That's the aromatase, that's what it does. That's how men can develop what's called gynecomastia which is where men start developing breast tissue. And guys who are on steroids have to watch out for that because you take a lot of testosterone, you make a lot of estrogen. But I think the big testosterone experts back in the day were recommending an estrogen level, estradiol level of about 25. And my estradiol level was a 24. So it seems that my body was doing a very, very good job of producing and regulating the testosterone and the estrogen. I'm not having to take external anti-estrogen pills or herbs to try to keep the estrogen down. I'm just doing what I do.
Dr. Smith:
But I can tell you that actually in the gym, the other day I was specifically noticing ... One of the things that happens to people but guys are going to be more familiar with this because guys mess around with testosterone and steroids more, is when you're on testosterone, the pumps, the muscle pumps that you get, are levels more intense than you would ever get when you're normal or less than healthy. And I was in the gym the other day going, "This is a crazy pump that I'm getting. This is like back when I was on testosterone. It's really wild."
Dr. Smith:
So I think that there is so much room for improvement in people. And like I said, all we're doing, all I'm doing ... I'm doing exactly what I have my people do. I test every six months. I do my hair testing more often than my normal clients do because I have a great haircut for it. And I have a special deal with the lab. But normally I do the hair tests about every, with blood tests, I do them every four to six months and we just adjust as we go.
Dr. Smith:
But yeah, the hormone stuff is going really well. And the women that do go and get their hormones tested note improvements along with their symptoms improve. So ...
Wardee:
So on your story, 10 years ago you used testosterone therapy to boost but then you were getting out of range so you stopped. You also didn't like-
Dr. Smith:
No, I did well. I reduced my dose to get more in range so that if I-
Wardee:
Okay.
Dr. Smith:
So I wouldn't get myself in trouble.
Wardee:
Yes.
Dr. Smith:
Yes.
Wardee:
But then you didn't really like it philosophically? For whatever reason, you stopped?
Dr. Smith:
I didn't like sticking a needle into my butt.
Wardee:
Okay.
Dr. Smith:
And I was also doing some hCG which is another approach to keep your own production normal. So I was using more than one med and I was having to inject hCG also. And it was just ... I just started going ... I looked at it and I went, "I don't want to do this for the rest of my life." And that happens to a lot of people. They're like, I don't want to have to wake up and have to put the cream on. It's like a prison. It's like a self-imposed prison. And I was looking at it after a while and I went, "You know this is ..." It's kind of nice, but I did notice my ex-wife at the time was like, "You're kind of being a jerk, like a lot." And I was going, "That's not normal for me." And I was kind of going, "I don't really ... That's not the way I want to be." And I noticed I was a little bit more short, maybe quite a bit more short with my daughter. And so I just started going, this is not the way that I want to be.
Dr. Smith:
And now, the amazing thing is, when I'm doing it this way, I have an amazing amount of patience. And everything's better in terms of frustration and anger and irritability. Everything's better because my liver's healthier and then my body's doing what it chooses to do rather than being forced into something. So yeah, it's a totally different situation.
Wardee:
Okay, great. So you've essentially done your own program for all these years and now you have quite healthy testosterone levels without supplementation?
Dr. Smith:
Yes, without supplementing testosterone. I do take a couple of supplements and we can talk about that.
Wardee:
Yes, but not hormone supplementation.
Dr. Smith:
But not hormones, yes.
Wardee:
Good, good clarification, right. Well that's great. So do you mind sharing with us a testimonial of a woman you've worked with who has had hormone issues resolved?
Dr. Smith:
Let me find it.
Wardee:
Okay.
Dr. Smith:
I had a couple pulled up.
Wardee:
Yeah, a couple is fine.
Dr. Smith:
A lot of times with my clients who are working with me, I don't do a lot of hormone tests because like I mentioned, hormone tests don't change what I do. They're showing me symptoms of hormones being out of balance. So let's see. Here's one. "I just sent in my hair sample to be analyzed so I have yet to work one on one with Dr. Smith but I've been independently doing his Vitamin A detox program", which we now call Love Your Liver Program, "for a little over two months and I've seen some interesting changes in that time. Mind you, I've been on a decade-long healing journey and have tried every diet, every modality you can name. The thing that I've noticed most is that my "body pleasure" seems to be increasing. I don't know how else to say it. My libido is going up and my orgasms are becoming more enjoyable. And my sleep is getting deeper." So that's just one evidence of hormones.
Dr. Smith:
For people who go on my YouTube page which is just Nutrition Detective, YouTube.com/nutritiondetective. I have a video on there of three fertility testimonials of women who I worked with and they went from infertile to fertile. One of them women, if I remember correctly, had had five years of unexplained infertility. And one of those years, she was working with me and at the end of that five-year time, she finally got pregnant again. But there's two other testimonials on that video.
Dr. Smith:
Here's a thyroid testimonial. "Well this is rather extraordinary, at least for me. Just got the latest TSH results. So 11 weeks ago, my TSH was 3.6," which is getting into, in my opinion, I would like it less than a 3 for sure. So anyway, "When the numbers start going in that direction, they usually continue to do so." She means up, which is not good. "They usually continue to do so without an increase in medication. This has been true for many years, since I've started paying attention. The TSH reading today was 1.69 which is better. My TSH has never gone the opposite direction." And she puts in parenthesis, "(The right direction), without an adjustment in meds." I'll be tested again in four months or so. People say my skin is glowing. Although having a bit of a tan probably contributes to that. I haven't worn foundation since being at the beach last month."
Dr. Smith:
Anyway, and that's ... They haven't worn foundation, that may go along with a lot of people who do the stuff that I suggest, that other people tell them they look younger. So they may be doing something like that.
Dr. Smith:
Okay. So this is about a guy, obviously is related to male hormone stuff but here's a guy writing about this. "I've already written you about this but I've had some benign prosthetic hyperplasia, AKA, prostate swelling for several years but not bad enough to be too concerned about. But over the last couple of years, I have developed a sensation of pressure and mild pain, prostatitis. I have tried different formulas." He probably means herbal formulas. "I also started having some pains in the pelvic/hip/thigh bones which was very concerning. It seems that around day 24 of the diet," he's talking about the low Vitamin A diet, the Love Your Liver Program, "I started seeing noticeable improvement in these symptoms. Now they are more sporadic and a prostate pressure and pain is almost gone."
Dr. Smith:
So on that note, I started developing ... My dad died of prostate cancer in his late 60s. So somebody might say I have a genetic tendency towards being weak, having a weak link in the chain in that area. I started developing prostate issues in terms of urinary issues in my mid-20s so that was a bad sign. I also took a drug called Ketoconazole, an antifungal as a teenager for a skin condition. Well if you go and you look up Ketoconazole on PubMed and you type in Ketoconazole and testosterone, you'll find all sorts of research showing that Ketoconazole damages your testosterone production. So I had prostate issues in my mid-20s. I know that that Ketoconazole damaged my testosterone. I won't go into the symptoms of that but I know that it damaged my testosterone as a teen.
Dr. Smith:
And then now, at age 46, I have no prostate issues or urinary issues and my testosterone is where we discussed earlier. So obviously those are all related to hormone type stuff.
Dr. Smith:
Okay, so this is kind of a long one, a little longer. But here we go. "I've been on Dr. Smith's hair mineral program for the past three years and it is the only program that has proven itself to work for me and my family members who are on it now also after my success.
Dr. Smith:
After 35 years of chronic health issues including fibromyalgia and hormone imbalances, I have given my best efforts to conventional medicine, traditional Chinese medicine, and acupuncture and numerous diets. Low-carb, alkaline, vegetarian, vegan, [inaudible 01:12:09] and everything in between. Custom supplements based on blood tests and even iridology." Which is the eye reading. I saw many well-intentioned specialists who had many answers that lead nowhere as well as doing a tremendous amount of research on my own. I was just leaving my "I give up phase" when I came to Dr. Smith with very little optimism and a literal long list of ailments.
Dr. Smith:
Slowly in some areas, and quickly in others, I began to see improvements and then began to cross each health issue off my list. My experience with the hair mineral analysis program," Hair mineral analysis is one thing I do. I also do some blood tests. "has been one of the two steps forward and one step back as my body has cycled through the healing process.
Dr. Smith:
Dr. Smith has walked me through each bump and celebrated with me over the successes that followed. Having confidence in my health provider and three years of consistent improvement makes it easy to continue. I have my list to look back on and a whole lot of hope to cross of the few remaining issues. I would encourage anyone who's considering Dr. Smith's program to jump in with both feet. His unique approach has been a worthwhile investment and his communication is top notch. Our family is the healthiest we've ever been."
Dr. Smith:
So anyway ... She included hormone imbalances in there as one of the symptoms that had gotten better, she just didn't go into specifics. But that's what I brought for that.
Wardee:
Neat, neat. Thank you for sharing those, Dr. Smith. And I will add that since working with you this year, which has been six months, the previous six years I had only increased, increased, increased, increased thyroid medication. Now in six months I'm down by one-third and hopefully more.
Dr. Smith:
Yay.
Wardee:
So that's really great. And I can share other testimonials with our audience as time goes on because I feel like I just barely started getting well.
Dr. Smith:
This is what we're trying to do. All we're trying to do is just bring things back the way they're supposed to be. But people will say, "Well people 100 years ago or 200 years ago or 300 years ago, didn't have to do what you're saying to do, Dr. Smith." And I go, "People hundreds of years ago didn't have tons of pokeys, tons of pharmaceuticals, tons of chemicals that they're ..." They didn't have cosmetics. They didn't have toxic cleaning supplies. There wasn't Roundup. There wasn't GMOs. There wasn't ... I mean rancid oils that they're eating.
Dr. Smith:
I mean really, the idea here, I just went over this in the livestream today. The world that we're in today, so if you have somebody broken, in a broken world, we are going to have to do things that people who back then who were not broken and were not in a broken world, we have to do more things to basically take the load off of the liver. So we have deficiencies in the soils. So if your soil's deficient, that means the plants are deficient. So if you're eating those plants, you're deficient. And if you're feeding plants to your meat animals, those animals are deficient. So everything's deficient up the chain. And then everything's toxic.
Dr. Smith:
And your liver, just being alive each day, you make toxins. Just like your car has an exhaust. We just ... By being alive, we make toxicity. Okay. So now you have that base level of toxicity that your body has to deal with every day just to stay alive. It's kind of like when people talk about the calories that you need, like your basal metabolic rate. Like you need X amount of calories to do your daily bodily functions. Or if you stay below that too long, you're going to shrink and shrivel and eventually die. Okay.
Dr. Smith:
Toxicity, you make a certain amount of toxicity per day. And then whatever you add to that, whether you chose to or whether it was forced on you, you then have to get rid of it. So if we want to bring that toxicity down and also get your minerals back up, well it'd be really good to know how much of the minerals you need and you respond positively to. But also, we have to do more things to reduce more toxic exposure than people back in the 1500s did. I mean this should just make sense to people. But people seem to be like, "But they didn't used to have to do this." And I go, "They're not living in this world today and ..." It'd be just like somebody who broke their ankle can't go jog. You can't just be like go out and exercise and jog. You broke your ankle. They need to do rehab exercises. And what we're doing is rehabbing their liver. So you need to take a load off of the liver so it can get back in shape the way it's supposed to be.
Dr. Smith:
When people hear a lot of the concepts that I go over, it starts to make sense to them. And then they go, "Oh, this makes sense." And I go, "Yeah, and it's not easy." The idea is you can just list out the ideas and say this looks simple. Just do A, B, C, D. But then they start going, "This is not easy. This is difficult." And you go, "Well ... "
Wardee:
But you always say just make one change at a time.
Dr. Smith:
Yeah. You can add-
Wardee:
You can't do it all at the same time. And then you can also measure better what impact a change has on you. Because you will either feel better, no change, or worse.
Dr. Smith:
Yes, yes. I do a lot of things which something is better than nothing. If people did one thing on my list of things, let's say, to avoid. That's better than they were doing before. And then there's perfection is the enemy of good. So people think they have to be perfect and do everything all at once when they first start and I go, don't do that to yourself. Just pick one piece, work on it for maybe a week or two and then pick the next piece. And use up ... I went to a woman's house and she had pounds of carrots in her fridge. Like bags and bags of carrots. And she started talking to me, she was like, "I got to get rid of all this, don't I?" I'm like, "You can do whatever you want. You can eat it up, you can use it up." And she actually went, "Well I'm just going to take it back, going to return it." That was like a Walmart thing. She was like, "I'm just going to take it back to Walmart and return it." And I was like, "Cool, get the money back. [inaudible 01:18:20] can get the money back.
Dr. Smith:
I remember, I was going through stuff at my house and I went through ... Everybody's gone through the diet phases where you're like, "Oh my gosh, I have to throw away all of this stuff." And then you either decide was I going to give it to somebody else? But then morals and ethics you're like, "Well wait, if I think it's a poison, do I want to give a poison to my neighbor? I don't know." So it's tough but I tell people, you can use up what you have. Work on the other things. Use up what you have. You spent good money on it. As long as it's not a Vitamin D supplement or a Vitamin A supplement. Those, just throw away. I tell people ... I don't make people throw stuff away. I mean I don't make anybody do anything. I tell them that everything you do is up to you. But we can throw things away and I'm to the point now where I'm like, "Yeah, just probably better to just throw that away."
Dr. Smith:
But anyway, yeah. We're just trying to get back to it. And people can go at any pace they want. Obviously, the more things you do, the sooner, there's good and bad to doing things quicker. One, the quicker you add things, in theory, and this makes sense, the sooner you can get better. The more toxins you take out and the more you get your minerals right, the sooner you can get better.
Dr. Smith:
But the reality of this process is, is when people are coming to me, usually they have decades worth of toxicity in them. Another saying I have is it's a poison on the way in and it's a poison on the way out. You cannot yank these poisons out too quick or you are going to feel like hot garbage because it's been these toxins floating around in your system that is what made you feel bad in the first place. And you've stored a lot of them. And so if all of a sudden you start doing things to yank them all out, they're out to play now. They're out in your system. And we have to, this is a big thing ... You've seen me, Wardee, on the network and talking to people in my office hours where I'm just constantly going, "Slow down. Chill out. Stop pushing so hard." It's kind of like if you think of people over-training with exercise. Can you exercise yourself into damaging yourself? Absolutely. Can you detox yourself into feeling like absolute dog poop? Yeah, you absolutely can.
Dr. Smith:
So a lot of the times, I'm sitting there trying to pull the emergency break on people and be like, chill out, go slower because it's too much for you right now and that's showing in your symptoms. And I explain it over and over again, the program. And still, people are sick and tired of being sick and tired. And they feel like I gave them a way out and so they slam the pedal to the metal and they just want to get it done and they ... Everybody always thinks they can handle the detox and I go, "Okay." I say, "Okay, come back to me when you're done." And they start going, "Can you make it stop?" And I go, "Yeah, stop doing all the things I told you not overdo." Anyway, it's a process. If people don't listen to their body, it's going to be a bad time. And if they don't listen to me and all the things I tell them, it's going to be a bad time. They're here because of the toxicity and getting the toxicity out is a rough process, if they don't listen. If they do it right, we can make it fairly smooth, but it's still not always going to be nice. Nothing good ever came easy, as they say.
Wardee:
That's right. That's right. Well thank you, Dr. Smith. So I'm sure people listening will want to know how to work with you. I will include links to Dr. Smith's YouTube channel, to his website. He does consultations, he also has his Love Your Liver Program which is the DIY version which I highly recommend for all the specifics because we can't possibly get into specifics, even to what forms of things Dr. Smith recommends because not all Zinc is the same. Not all potassium is the same. Not all magnesium's the same, et cetera.
Wardee:
But what would you add to that list of how people can work with you?
Dr. Smith:
The main things, I have ... If you're looking for me around the internet, just look for Nutrition Detective, you'll generally find me. Twitter, Facebook, Instagram, YouTube is Nutrition Detective, too.
Dr. Smith:
So for people who work with me where they do the blood tests, and the blood test is like four tests. You're used to going to your doctor and getting 40 tests or whatever, and I do four. And we do the hair test and then there's the consultation and support. That's at nutritiondetective.com. That's where you can find that under the consultation link. And people who work with me directly, who work with me on the consultation stuff, they get access to the Love Your Liver Program, the do it yourself program, because that's all the dietary stuff and the toxin avoidance that I need everybody to do.
Dr. Smith:
For people who maybe aren't ready to work with me or just want to do it on their own, that's the Love Your Liver Program. That's members.nutritiondetective.com. And that's where they can go if they just want to do that. Those are the two main ...
Dr. Smith:
And then on the nutritiondetective.com, I do make a couple of supplements. Those are, when people are wondering what supplements was I taking when I'm talking about the testosterone stuff and the other stuff that I use with my clients, I do use more supplements than are on my website. I only have two things so far but we got the Lactoferrin and the [inaudible 01:23:48] minerals. Those are a big part for a lot of people. We're working on more stuff as we speak. But yeah, so those are the three things that I mainly do right now.
Wardee:
Well thank you so much, Dr. Smith. We appreciate your time and your care and your wisdom. And I hope everybody listening has gotten a lot out of it, I sure have. And if I would say anything, it's basically that everything you have told me works. I have felt benefit from everything you've told me. From your program, and working with you individually too. So I'm very, very thankful and I hope others will avail themselves of you, as well.
Dr. Smith:
That's the goal. That's all I'm trying to do is help people get better.
Wardee:
And it's empowering because I also feel like I'm working with myself, my own body, at a level I haven't before in my life and I'm in my 40s and it's about time. So thank you and God bless you and everyone just be sure to check out the transcript and links for more information. You can take this as far as you want it and I'll be praying for you all, too.
Sign up to receive email updates
Enter your name and email address below and I'll send you periodic updates about the podcast.
The Background
In our interview, Dr. Smith shared that he has spent his career looking for the “skeleton key” to unlock the root cause behind our modern-day chronic diseases. Although treatments that help symptoms are not necessarily a bad thing, he explains that he wanted to figure out what was causing the problem in the first place — perhaps by removing a toxicity or addressing a deficiency — so the body can heal itself.
He asked questions like: “What are so many of us doing wrong so that we have chronic diseases? Could the different diseases showing up in different ways in different people be related to a common cause?”
Symptoms of Hormonal Imbalance
The symptoms of hormone imbalance are wide and varied. Here are just a few:
- fatigue
- weight gain
- pre-menstrual syndrome (PMS)
- painful and/or heavy menstruation
- insomnia
- constipation and/or other digestive complaints
- acne and other skin conditions
- infertility
- mood swings
- bone loss and/or osteoporosis
- aches and pains
- low libido
- sexual dysfunction
- muscle weakness
- headaches
- hair loss
- aging skin
- insulin resistance
- and more…
Why do we have hormone problems?
Dr. Smith believes that many hormone imbalances can be traced back to too much estrogen. Whether by consuming too many estrogens through diet and lifestyle, and/or by consuming substances that increase the activity of a certain enzyme called aromatase which converts testosterone into estrogen in the body, hormonal imbalance results.

Vitamin A
As shared in our Healthy Diets eCourse lesson on the Low Vitamin A diet (found in Traditional Cooking School’s Bible-based cooking program), Dr. Smith does not believe that Vitamin A is a true vitamin, but rather is a plant poison derived from carotenoids. The research shows that Vitamin A stimulates aromatase activity, which means that it prompts the body to take a hormone that it wanted (testosterone) and turn it into estrogen instead.
In studies, scientists have used retinoic acid (the active form of Vitamin A) to treat hypercortisolism (Cushing’s syndrome). Dr. Smith asks the question: If you can drive hyperactive adrenals back down to normal with Vitamin A, what happens when you have normal adrenals and you consume too much Vitamin A? Wouldn’t that induce adrenal fatigue?
He explains that some of the Vitamin A in foods eventually turns into retinoic acid in the body. Many women apply retinoic acid to their faces in the form of skincare products. Many, many superfoods and supplements are high in Vitamin A.
So Vitamin A toxicity is a key problem behind hormonal imbalances.
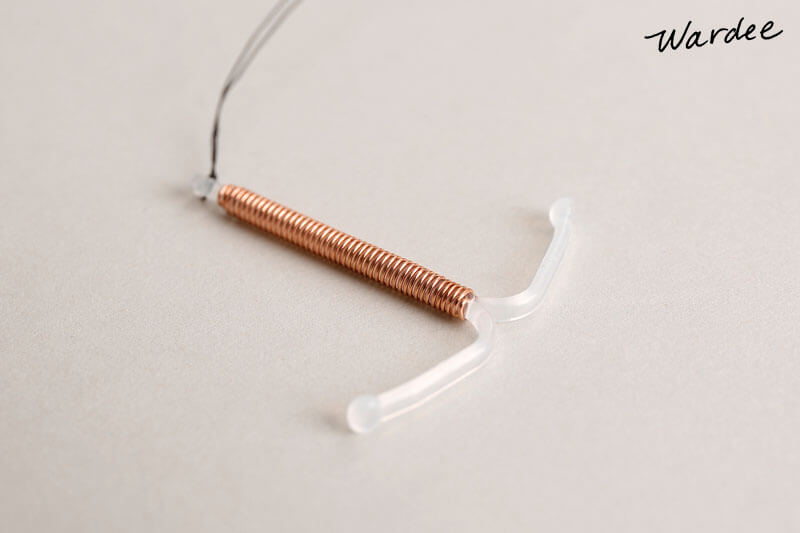
Copper
Many other toxins are also estrogenic: xenoestrogens (such as plastics), phytoestrogens (plant estrogens such as unfermented soy), and copper.
Dr. Smith explains that we are exposed to more copper on a daily basis than we’d originally think. Chocolate is high in copper. The pipes in our houses are often copper, which means that when we shower in hot water, we are absorbing copper (which is measurable in hair analysis tests!). For those on birth control, birth control pills raise the levels of copper (and Vitamin A) in one’s bloodstream, and of course the copper IUD is a little copper wire stuck in one’s uterus to prevent pregnancy.
Copper is anti-fertility, yet fertility is health, and health is fertility. If you damage your fertility, whether you think it’s temporary or not, you are damaging your health. If you wanted to think in terms of testosterone and estrogen, copper is extremely estrogenic and zinc is pro-testosterone. Everybody needs testosterone — not just men! In fact, both men and women need some estrogen and some testosterone. The problem is, in our world today, everything is radically geared towards estrogen with excess copper, excess Vitamin A, not enough zinc, plastics, etc. Many toxins are very estrogenic.
Additionally, our soils are deficient in zinc and molybdenum, which are the antagonists to copper and Vitamin A. So you’re getting too many estrogens and not enough of the critical minerals to regulate estrogens.
If we take in more estrogens than we can get rid of in a day, they are stored in our fat and in our liver. As they accumulate, your problems will slowly get worse. It’s just math, as they say.
Why is estrogen bad?
According to Dr. Smith, estrogen causes tissue growth such as body fat. This is why women, who naturally have more estrogen in men, are also naturally curvier and softer. He continues…
Yet, if estrogen gets out of control, it can start growing tissue in other areas, too. One area of the body, especially in women, that is very controlled by estrogen is the breasts. We have an epidemic of breast cancer. We have epidemic of excess estrogens. This all seems to fit together. And there’s lots of other sexual organ cancers and tumors like fibrocystic disease. When you think of tissue growth, especially out-of-control tissue growth, think estrogen.
As an example, when I mentioned before that copper is very estrogenic, you can see in cancer research that tumors are higher in copper than the other tissues around them.
This is true for men and women: When people get too much estrogen, they start gaining body fat. Body fat contains aromatase. When any of the testosterone you’re making hits that body fat, it gets turned into estrogen. Estrogen makes more body fat. And the vicious cycle continues.
How to Balance Hormones Naturally
Simply put: Dr. Smith believes the best way for everyone to balance their hormones is to reduce their toxic load, and become more “mineral replete”. He says…
In my Love Your Liver program, where I lay out my diet and toxin avoidance recommendations, I suggest certain supplements for both men and women. When people work directly with me, I provide blood and hair testing as well so that we can fine-tune the supplement recommendations so they are getting exactly what they need for their bodies, taking into account their medical history, etc.
The major minerals I suggest for everyone are magnesium, potassium, zinc, selenium, and molybdenum. If I am working with someone specifically, then we take into account what their tests say, their body weight, and their history of how they’ve reacted in the past. I do not test for hormones because hormone testing is very expensive — hundreds of dollars for just a couple tests — and instead, we can look at their symptoms to learn the state of their hormones.
Over time, as people remove toxins and become replete in the nutrients they were deficient in, they start needing less supplementation. They feel better with less, whereas in the beginning, they felt better with more. It’s a process, we re-assess periodically, and that’s the way it should be, in my opinion. To succeed in my program, people have to take responsibility and actually watch how they’re feeling.
Hormones as a symptom is a different concept to many. People think of hormones as the most powerful things in our bodies, the most important, at the top of the pyramid. I think of hormones as at the top of the pyramid, sure, but that means they are built on a foundation of everything below — toxins, minerals, protein and other macros, lifestyle choices like exercise, etc.

Are there different recommendations to balance hormones for men vs. women?
Dr. Smith shares…
Toxins are toxins. I don’t have different approaches for men and women because there aren’t male-specific toxins versus female-specific toxins. However, it has been shown that polyester in men’s underwear reduces testosterone and sperm count. So wear cotton underwear, basically. I would guess this probably extends to women, too!
What about menopause?
According to Dr. Smith,
The thing to remember is that the ovaries are not the only hormone producers in the body. The uterus makes sex hormones, the adrenal glands make some sex hormones. Body fat makes estrogen, which is a sex hormone. When women go through menopause, the ovaries may stop producing, but the rest of their body should still be making hormones… if they are healthy. Now, a full hysterectomy would be different since the other sex organs that also make hormones, such as the uterus, would be removed.
If fertility-suppressing toxins such as Vitamin A and copper are removed, women going through menopause have an easier time of it because their sex hormones are still being produced by the rest of their body. I have treated a woman whose osteoporosis reversed so that her body was making bone again. I have treated women who were in menopause yet started cycling again when their toxicities and deficiencies were addressed. Remember, fertility is health! Cycling is youthful.
In fact, young women have an easier time of pregnancy and delivery, too, and their children are healthier when they follow my program!
Why didn’t people have to do this hundreds of years ago?
Dr. Smith explains that people hundreds of years ago didn’t have pharmaceuticals, cosmetics, toxic cleaning supplies, GMOs or RoundUp. They didn’t eat rancid seed oils. People like us who are broken in a broken world will have to behave differently than people back then who were not broken and didn’t live in a (as badly) broken world. So too, deficient soils mean deficient plants mean deficient animals… mean deficient people! So in our modern-day world we have to deal with more toxins and more deficiencies.

Does hormone replacement therapy work to balance hormones?
Dr. Smith used to give hormone replacement therapy (HRT) in his practice, but eventually realized that it is flawed because it treats the symptoms, not the cause. Even bio-identical hormones, which are certainly better, do not treat the root cause.
He explains that if you’re taking HRT but you’re not addressing your mineral deficiencies and/or you are eating the standard American diet, then the hormones function as a giant band-aid while you continue to get more toxic and more deficient over time. This is especially apparent when people try to get off their hormones, but feel worse than when they started.
Dr. Smith clarifies that there’s nothing wrong with symptom relief, but what is driving the symptoms in the first place has to be resolved or very likely it will just fester and worsen over time.
He shares an example that both men and women can relate to…
People are going to the doctor saying, “I have these symptoms, doc.” And they test them and they say, “Okay, we looked at your symptoms, we tested you, you need X amount of estrogens.” The E1, E2, E3, whatever they’re doing. Or, “You need so much progesterone and maybe we’ll add a little testosterone in the mix.” And the patients start using it. Sometimes they feel worse. Most of the time they feel great and they go, “This is great. I got my libido back and everything’s working better.”
They keep using it, and at follow-up appointments, the doctor’s saying, “Your labs are good, your labs are good. Let’s raise you here. Or, let’s lower you here.” Even if they’re using bio-identical hormones (which are better), hormone therapy still treats the symptoms.
Let’s say the low hormones were caused by a toxicity or a nutritional deficiency. Over time, if it’s not addressed, the problem is just going to get worse, despite the hormones. What happens when the patient goes back to the doctor? Well, the person’s saying, “My symptoms are coming back, doc.” And the doctor’s going, “Oh yeah, your hormones are dropping a little bit. Let’s give you some more.” The person may feel a little better but they never feel as well as they did in the beginning during the “honeymoon phase”.
With guys, you give them testosterone, you take them up fairly high in the normal range. And the guy comes in and he’s like, “Hey, doc, I feel good but I’m not functioning as well. Can we bump it up?” The doctor will keep raising it until they get right to the edge of the okay range or maybe a little bit above it and then has to stop. It’s not good for their license to be caught raising guys above the normal range. So they say, “Look, I don’t know why you don’t feel as good as you did before but I can’t give you any more.”
This is a common thing because the body adapts. External hormones are not the same as internal hormones.

Dangers of hormone replacement therapy
As we become more aware of our toxic load and how much our liver does to process toxins and keep our body healthy, it becomes apparent how hard our liver has to work to keep up with HRT. According to Dr. Smith…
Nutrients, toxins, hormones, etc. are absorbed from the digestive system into the portal venous system. The portal vein goes right to the liver where the liver processes them to let good things into the body, and keep bad things out. This is called first pass metabolism.
During first pass metabolism, if you are on HRT, your liver has to process hormones*. Compared with other molecules, hormones are giant and intricate. They make more work for your liver, which may already be working hard keeping up with other modern-day toxins. If you’re taking in more than your liver can get rid of, you’re going to start accumulating hormones instead. Your body doesn’t want too many hormones in your bloodstream so it stores them in fat. This means, even if people get off of hormones, they have potentially months or even years of hormones left in their fat cells to get rid of.
Bio-identical hormones are much better than synthetic hormones but they are still a load to your liver. The more load you add to your liver over time, the more potential liver injury you cause, the slower your liver runs, and the less hormones you clear. Which means it becomes easier to accumulate them and then store them.
Anything taken by mouth will be hardest on the liver, because the liver has first pass at it. On the other hand, creams, injections, pellets, etc. bypass the liver and enter the bloodstream directly. You take control of your detox away from your liver, but in theory, this could potentially cause more problems because the hormones are doing what they do before your liver has a chance to say yea or nay.
Everything we take in orally is a load for the liver. That’s why we’re trying to take in only the things that we need, and why I try not to over-supplement people. The toxins, the hormones, the extra pills and supplements — it all adds up and the liver bears the brunt.
In Chinese medicine, the liver is the seat of anger and frustration. This is why they talk about “roid rage”. The more damaged your liver, the more angry and irritable a person tends to become, especially men. Women tend to be more weepy, depressed, and anxious.
*Funnily enough, the liver will destroy a lot of the hormones people take orally, which is why doctors compensate by giving higher oral doses.
What is the best way to get off hormone replacement therapy?
This is what Dr. Smith would consider doing with an active patient under his care:
Generally with hormones, if you don’t want a big crash, you’ll need to wean. Now, weaning is done at an individual’s rate. I never tell anybody how fast they have to wean off of something. But one of the first questions I always ask people is “Did the hormones change how you felt?” And honestly, you would be surprised at how many people are like, “They didn’t do anything for me.” And I go, “Well then you should be able to just stop.” If some people say, “No, I’ve felt bad since I started on hormones,” then they can stop, and the bad symptoms will go away.
If weaning is necessary, then I have my patients do a test run. They drop their dose by half, give it a week or two, and see how things change. After a week or two, they can determine whether or not they want to drop their dose again.
Even if my patients decide they’re not ready to stop the hormones, it’s okay. People can use all sorts of crutches. And over time, I might say, “Would you feel comfortable with trying less?” And the way I am with my clients, the client is either just like, “Sure, yeah, I’ll try less.” Or maybe they’ll say, “I already tried less. I wasn’t quite ready for it.”
If somebody was on synthetic hormones, I would first move them to bio-identicals, then we would try slowly weaning from there.
Weaning off thyroid hormone…
With thyroid hormone, I tell people not to change their thyroid hormone until they start getting hyperthyroid symptoms. This is because they are already managing their symptoms with thyroid hormone. Well, as we start getting them better, their natural thyroid hormone production is going to increase. Now they’re over-medicated. So I educate them on hyperthyroid symptoms so that if and when they suddenly experience these symptoms, they know to cut their dose of thyroid hormone by half. In a day or two, if the symptoms drastically go back to normal, we very simply know they were over-medicated because we were actually fixing their thyroid.
Some people think once you’re hypothyroid, you’re always hypothyroid. That’s not how things work in my world. Unless you’re missing the glands that make the hormones or they’ve been so destroyed that they make nothing, we can absolutely improve what your body is making by repairing the underlying cause(s). This takes time, however. It’s a marathon, not a sprint.

Dr. Garrett Smith’s Story
In 2012, my testosterone was 600. This was after having only one kid. Then I got on testosterone and raised it outside of the high end of normal, to 1200 or 1300. I know what being on steroids feels like — I was bigger, more muscular, but fatter too. And I was more irritable. Finally, I decided to stop. I didn’t want to inject medications for the rest of my life, and I didn’t want to be irritable with my wife and daughter.
Now, about ten years later, I’m 46 with testosterone at 900. For a 46-year-old man who runs small business with two kids, that’s really good! I don’t take testosterone or use testosterone-boosting herbs or any of the things that internet people are trying to sell. I’m more muscular than I was in college. I have lower body fat than I’ve had probably since late teens, early 20s. So everything in my system is running better than it used to.
My estradiol level is 24. Testosterone experts back in the day were recommending an estrogen/estradiol level of about 25. It’s something that men supplementing with testosterone have to watch out for, because aromatase turns a lot of the testosterone into estrogen. If it’s too much estrogen, men can start developing breast tissue. A level of 24 means my body is doing a very good job of producing and regulating both testosterone and estrogen. I’m not having to take external anti-estrogen pills or herbs to try to keep the estrogen down. I’m just doing what I do — exactly what I have my patients do.
My dad died of prostate cancer in his late 60s. As a teenager, I took an antifungal drug called Ketoconazole for a skin condition. Unfortunately, there’s research that shows that Ketoconazole damages your testosterone production. As a result of that and my genetic tendency toward prostate issues, I started developing urinary issues in my mid-20s. That was a bad sign. 20+ years later, I have no prostate or urinary issues.
Testimonials
A female patient sees improvement in her sexual health:
“I just sent in my hair sample to be analyzed so I have yet to work one on one with Dr. Smith but I’ve been independently doing his [Love Your Liver program] for a little over two months and I’ve seen some interesting changes in that time. Mind you, I’ve been on a decade-long healing journey and have tried every diet, every modality you can name. The thing that I’ve noticed most is that my “body pleasure” seems to be increasing. I don’t know how else to say it. My libido is going up and my orgasms are becoming more enjoyable. And my sleep is getting deeper.”
One of Dr. Smith’s patients who takes thyroid medication sees her labs improve for the first time:
“Well this is rather extraordinary, at least for me. Just got the latest TSH results. So 11 weeks ago, my TSH was 3.6 [which is too high, Dr. Smith would prefer to see it less than 3]. When the numbers start going up, they usually continue to do so without an increase in medication. This has been true for many years, since I’ve started paying attention. The TSH reading today was 1.69 which is better. My TSH has never gone the opposite direction (the right direction) without an adjustment in meds. I’ll be tested again in four months or so. People say my skin is glowing. Although having a bit of a tan probably contributes to that. I haven’t worn foundation since being at the beach last month.”
A male patient is reversing pain and prostate swelling:
“I’ve already written you about this but I’ve had some benign prosthetic hyperplasia, AKA, prostate swelling for several years but not bad enough to be too concerned about. But over the last couple of years, I have developed a sensation of pressure and mild pain, prostatitis. I have tried different formulas. I also started having some pains in the pelvic/hip/thigh bones which was very concerning. It seems that around day 24 of the [low Vitamin A diet] I started seeing noticeable improvement in these symptoms. Now they are more sporadic and [the] prostate pressure and pain is almost gone.”
A female patient begins healing 35 years of chronic health issues:
“I’ve been on Dr. Smith’s hair mineral program for the past three years and it is the only program that has proven itself to work for me and my family members who are on it now also after my success. After 35 years of chronic health issues including fibromyalgia and hormone imbalances, I have given my best efforts to conventional medicine, traditional Chinese medicine, and acupuncture. [I’ve tried] numerous diets [including] low-carb, alkaline, vegetarian, vegan, Weston A. Price, [c]ustom supplements based on blood tests and even iridology. I saw many well-intentioned specialists who had many answers that lead nowhere as well as doing a tremendous amount of research on my own. I was just leaving my ‘I give up phase’ when I came to Dr. Smith with very little optimism and a literal long list of ailments.
Slowly in some areas, and quickly in others, I began to see improvements and then began to cross each health issue off my list. My experience with the hair mineral analysis program has been one of the two steps forward and one step back as my body has cycled through the healing process.
Dr. Smith has walked me through each bump and celebrated with me over the successes that followed. Having confidence in my health provider and three years of consistent improvement makes it easy to continue. I have my list to look back on and a whole lot of hope to cross off the few remaining issues. I would encourage anyone who’s considering Dr. Smith’s program to jump in with both feet. His unique approach has been a worthwhile investment and his communication is top notch. Our family is the healthiest we’ve ever been.”
Where to Go from Here
Balancing hormones by removing toxicities and becoming more “mineral replete” is a simple concept, but Dr. Smith warns that it is hard to execute. Nothing worth doing is easy! And yet, for those of us who have been struggling health-wise for years, our day-to-day is already hard, so at least this offers a glimmer of hope at the end of the tunnel!
Below you will find links to Dr. Smith’s website and YouTube channel where you can find many resources, including diet and supplement recommendations, to get you started. You can also check out Lesson 8 of our Healthy Diets eCourse (Traditional Cooking School’s Bible-based cooking program) where I interview Dr. Smith about the Low Vitamin A diet he teaches as a foundational part of his Love Your Liver program.
Dr. Smith recommends making one change at a time. Something is better than nothing. Detoxing too quickly from (possibly decades of!) toxicity can feel unbearable, so take it slowly. He often says: “It’s a poison on the way in, and it’s a poison on the way out.” Meaning, the toxins in your system made you feel badly in the first place, but at least your body stored them. Once you start getting rid of them, they are out wreaking havoc again as they leave!
So, don’t overdo it, but remember that the more toxins you take out and the more you get your minerals right, the sooner you can balance and heal your hormones. I hope this information will help you to live a fuller, healthier, and beautiful life!
Links
- Three fertility testimonials from Dr. Smith’s patients (on YouTube)
- How birth control pills ruin your health (on YouTube)
- Dr. Smith’s reviews his recent hormone test results (on YouTube)
- Love Your Liver program (included free if you do a consult with him)
- Nutrition Detective YouTube channel
- Dr. Smith’s consultation program (individual or group options)
- Dr. Smith’s supplements
- Traditional Cooking School’s Bible-based cooking program (Healthy Diets eCourse Lesson 8 is on the Low Vitamin A diet)





Leave a Reply